Hormone replacement therapy, or HRT, is a relatively common medical treatment used in many contexts. Despite what many may think, this is not a new or experimental practice, nor is it exclusive to transgender individuals. Hormone replacement therapy has been used for over half a century, starting its use in the 1960s and is widely popular in treating menopause in AFAB (assigned female at birth) patients.
In this page, we will cover how HRT can be used in AMAB (assigned male at birth) patients for gender affirmation, a type of HRT known as feminizing HRT. Feminizing HRT can have profound effects even on patients who are post-puberty, and has the potential to significantly improve quality of life for transfeminine individuals.
How to get HRT
Official transition routes for gender/sex reassignment therapy vary by country and the healthcare standards applicable there. Requirements for it can go as high as psychological evaluation for a diagnosis of gender dysphoria to as low as merely giving informed consent. You need to research available options in your country to find the most accessible method for you. Try strict searching "trans" "healthcare" "[your country]" see if you can connect with anyone who transitioned from where you live.
- South America http://redlactrans.org.ar/site/
- USA https://www.plannedparenthood.org/get-care/our-services/transgender-hormone-therapy
- Canada https://cpath.ca/en/
- Australia https://auspath.org.au/
- UK https://www.gendergp.com/help-centre/gendergp-service-costs/
- Europe https://tgeu.org/trans-health-map-2022/
For other countries you should try looking at this map of international transgender resources or this reddit page.
Alternatively you can get your own medication online and administer it yourself. Order from here https://diyhrt.market/stores/ and use this guide.
What can HRT do for me?
Feminizing HRT seeks to lower a patient's testosterone level and raise their estradiol (AKA E2, the most biologically active estrogen) level, targeting levels similar to those of an average cisgender woman. Feminizing HRT can also involve many other medications, such as antiandrogens or progestogens. The end result is overall feminization of the body and its secondary sex characteristics. Changes may include healthier skin, female fat redistribution throughout the body, and breast growth.
| Effect | Permanence | Expected Onset | Maximum effect |
|---|---|---|---|
| Body fat redistribution | Reversible | 1-2 months | 2-5 years |
| Decreased muscle mass | Reversible | 1-2 months | 1-1.5 years |
| Decreased skin oiliness | Reversible | 1-2 months | 1-1.5 years |
| Skin softening | Reversible | 1-2 months | 1-2 years |
| Decreased libido | Reversible | days-weeks | weeks-months |
| Less or no random erections | Reversible | days-weeks | weeks-months |
| Erectile dysfunction* | Reversible | days-weeks | weeks-months |
| Breast development | Irreversible | 2-6 weeks | 2-6 years |
| Decreased testicular volume | Variable | 1-3 months | 2-3 years |
| Decreased sperm production | Variable | 2-6 weeks | 1-3 years |
| Decreased semen volume | Veriable | 2-6 weeks | 1-3 years |
| Slowing of body & facial hair growth** | Reversible | 1-3 months | 6 months-1 year |
| Voice changes*** | N/A | none | none |
| Reversal of male pattern hair loss**** | Reversible | 1-3 months | 1-2 years |
*: Most individuals do not experience erectile dysfunction.
**: HRT will slow down body and facial hair growth, but only laser or electrolysis can stop it entirely.
***: Feminizing HRT does not cause an effect on an individual's vocal folds.
****: Male pattern hair loss can be prevented with HRT, but reversal of hair loss is rare.
So, what should I take, and how much?
Again, the goal of feminizing HRT is to bring your hormone levels (estradiol and testosterone in particular) from your current male range to that of a healthy cisgender woman. On top of this, there are some medications and other hormones we will cover, such as antiandrogens, progestogens, and other niche or specific medications, including hair loss treatments and more experimental methods for feminization.
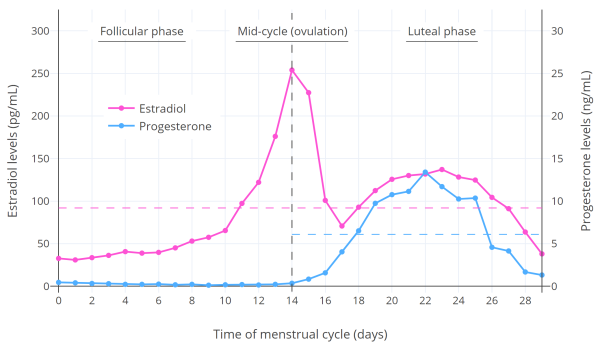
Before we talk about specific medications, you need to have a basic understanding of the target hormone levels. According to the Journal of Clinical Endocrinology, for feminization to be effective you should be within the levels of a premenopausal female:
100-200 pg/ml estradiol & <50 ng/dl testosterone.[2]
with some variation depending on the method you take your levels should approximate the menstrual cycle:
higher levels do not cause greater feminization and may have even have a counterproductive effect as estrogen may have an inhibitory effect on cell proliferation at a higher level. [3]
Blood tests are the only effective way to measure these levels and are extremely important in minimizing the risks of HRT and maximizing its effectiveness. We will talk about how to manage being in a situation where you cannot access bloodwork. This is not impossible, but we highly recommend against it.
The most efficient method of administering estradiol is via injecting a solution. Pills are much less efficient, and patches and gels are generally somewhere between the two in effectiveness.
Injection monotherapy
Estradiol is the most biologically active estrogen and heavily contributes to feminization. On top of this, it contributes to the suppression of testosterone.
In estradiol-only HRT, also known as monotherapy, estradiol alone provides both feminization and suppression of testosterone into female ranges. This is possible because of estradiol's suppressing effect on testosterone by itself at high enough levels. Monotherapy removes or reduces certain potential risks and side effects that may be caused by antiandrogens used to help with testosterone suppression, but usually requires more estradiol and is much harder to achieve with specific routes of administration such as oral or transdermal.
Injections are an excellent example of an ROA suitable for monotherapy. It is rare for someone to be unable to achieve proper levels through injections. There are several common esters (chemical variations) used for injectable estradiol. These include valerate, cypionate, enanthate, and less commonly, undecylate.
Effective dosages vary wildly from person to person, though there is a reasonable range of starting dosage. If you have access to bloodwork, finding your dosage should be simple. Start with a sane dosage that works for most people, which we are about to cover now, and get a blood test just before the next injection at the "trough", or lowest level in your cycle, after a few weeks.
The most significant difference between the esters is their stability, or biological half-life. Estradiol valerate has a half-life of 4-5 days[4], cypionate 8-10 days[5], and enanthate 5-7 days[6]. However, research suggests that enanthate's peak comes later than cypionate, so it is generally best to treat them the same. Valerate is the most common pharma-grade ester in the US due to the cypionate shortage. Enanthate is the most common ester found in homebrew due to its incredible stability, and is prescribed in some countries.
| Ester | Elimination Half life | Starting dosage | Maximum time in between injections |
|---|---|---|---|
| Valerate | 4-5 days | 3.5mg/5 days | 7 days |
| Cypionate | 8-10 days | 4mg/7 days | 14 days |
| Enanthate | 5-7 days* | 4mg/7 days | 14 days |
These dosages must be adjusted based on bloodwork. It is possible to extend the time between your dosages from every 5 days with valerate up to every 7 or even every 2 weeks with cypionate or enanthate (however 10 days is a much safer bet).
This lovely simulator can be helpful if you are trying to approximate your dosage. It averages the estradiol level of many people on injections into a graph based on several studies, but it is important to remember that it can be highly inaccurate on an individual basis and should not be used as a replacement for bloodwork. I was on a prescription dosage of 8mg estradiol valerate, with my trough (right before the next injection) over 650 pg/ml; the simulator's estimate is just below 200 pg/ml.
No access to bloodwork
Dosing your HRT without bloodwork may be unsafe and could lead to complications; it is highly recommended that you get bloodwork if at all possible. We cover how to get blood tests even without a doctor or prescription HRT here, but if you absolutely cannot get bloodwork, all you can do is take a reasonable dosage and hope it works. Some things to look out for to guess if your dosage is working are breast growth, nipple sensitivity (sensitivity is rarely constant and can go away for long periods), and general changes HRT is supposed to have on a person.
How to do an injection
Injecting medication is a relatively straightforward process but easy to screw up. Learn how to do a proper injection here.
Antiandrogens AKA testosterone blockers
Antiandrogens are medications that counteract the effects of androgens—male sex hormones such as testosterone or DHT. High-dose estradiol is an effective antiandrogen, but for some patients it may be very hard or impossible to get proper levels without an additional antiandrogen. Common antiandrogens for feminizing HRT are cyproterone acetate, spironolactone, and bicalutamide. These medications all work in different ways to suppress androgens. Compared to injection monotherapy, the accompanying dose of estradiol is usually lower when an additional antiandrogen is used.
Bicalutamide is an antiandrogen also used to treat prostate cancer by blocking the effects of testosterone, which in turn slows or stops the growth of cancerous cells.[7] This testosterone blocking effect is desirable in feminizing HRT, and as such, bicalutamide is a common choice of antiandrogen. It is commonly dosed at 25-50mg/day. Keep in mind when taking bicalutamide that it does not block testosterone production; testosterone blood levels may significantly increase.[8] Instead, it prevents testosterone from attaching to its receptors. Although you still have it in your blood, on a proper dosage you will not experience any androgenic effects.
Cyproterone acetate is a progestin with androgenic and progestogenic effects. Like bicalutamide, it is used in treating prostate cancer. It is not approved for use in the US but is a standard option in many other countries. Even without estrogens, cyproterone acetate reduces testosterone levels very efficiently.[9] Cyproterone acetate is most effective in daily doses of 10mg, though most patients take 12.5mg because they split one 50mg pill into 4 pieces.
Spironolactone is one of the most common antiandrogens used in feminizing HRT. It is also a diuretic, and as a result may cause you to urinate more often. Spironolactone helps your body retain potassium, so you should be mindful when consuming potassium-rich foods while taking it.[10] Spironolactone is a weaker antiandrogen compared to the two above, but is relatively safe and commonly prescribed in the US. It is typically dosed at 100-200mg daily.[11]
Finasteride is an antiandrogen used in treating prostate inflammation and male pattern hair loss. It inhibits the conversion of testosterone into its more potent form, DHT (dihydrotestosterone).[12] Finasteride does not lower testosterone significantly and should not be used as a replacement for the antiandrogens above, although it is an effective treatment for hair loss.[13]
Before taking any antiandrogen, it is important to understand the safety profile and possible side effects. Be sure to monitor yourself for side effects when starting a new medication, and consult your doctor if you experience any serious issues.
Oral or sublingual estradiol
If you cannot handle performing injections, or are unable to source injectable estradiol, oral or sublingual estradiol tablets are another option. Usually taken with an antiandrogen, estradiol tablets are commonly composed of one of two common forms of estradiol: ethinyl estradiol or estradiol valerate. They are both very similar[14], with only minor differences in their half-lives. Ethinyl estradiol has a slightly longer half-life, and 1mg of estradiol valerate orally equals 0.76mg of ethinyl estradiol.[15] Overall, you don't have to be super picky, and either one is likely to be just as effective.
While oral estradiol is administered simply by swallowing the tablet, sublingual ROA for estradiol is administered by placing the tablet under the tongue, where it is absorbed through the dense blood vessels found in the connective tissue. Relatively new but very promising, sublingual dosing achieves much higher levels when compared to oral dosing, and avoids passing through the liver, which is safer and reduces the risk of blood clots. However, it generally requires more frequent dosing, as it has a much shorter half-life.[16]
| Route of Administration | Low/Initial Dosage | Maximum Dosage | Frequency |
|---|---|---|---|
| Oral | 2-4mg/day | 6-8mg/day | 1-2x daily |
| Sublingual | 1-2mg/day | 4-6mg/day | 2-3x daily |
The dosages above should be divided throughout the day according to the frequency, not multiplied.
Transdermal estradiol
Transdermal estradiol is another ROA for feminizing HRT. It is one of the safest methods, prescribed especially in older patients or those with risk factors such as tobacco use. Typically, a patch or gel is applied to the skin, but less commonly, a spray form of estradiol can be used. A common downside of transdermal estradiol is that many find it hard or infeasible to achieve cisgender hormone levels; antiandrogens are often used in conjunction if testosterone cannot be suppressed by the estradiol alone.
Patches can come in dosages up to 100mcg released per day; often, it takes wearing multiple 100mcg patches at a time to remain within target ranges or effectively block testosterone, with a typical dosage being 100-400mcg per day. Patches must be changed weekly or twice weekly.[11]
Dihydrotestosterone
Dihydrotestosterone, or DHT, is an androgen that affects the growth of the prostate, along with being the primary cause of male pattern hair loss. Depending on your regimen, you may want to take a DHT blocker to prevent hair loss. Read more on hair loss here.
Progesterone
The effects of progesterone in transgender women is very controversial. Some say, that there are no effects at all, while others believe that there are improvements in permanent fat distribution. There are many articles & studies about this topic, and we will not teach one specifically. You can go check the progesterone page for more information on individual theories.
The TLDR is: it is known that progesterone has anti-depressant effects, and allows water weight to move to more feminine areas. Due to a lack of studies, we cannot definitively say any more information.
Experimental HRT
There are a few somewhat common medications—pioglitazone or estrone, for example—that some people claim help with feminization. This section will probably take a while to write and research. For now, it is empty.
- ↑ Mayo clinic: Feminizing hormone therapy https://www.mayoclinic.org/tests-procedures/feminizing-hormone-therapy/about/pac-20385096
- ↑ Wylie C Hembree, Peggy T Cohen-Kettenis, Louis Gooren, Sabine E Hannema, Walter J Meyer, M Hassan Murad, Stephen M Rosenthal, Joshua D Safer, Vin Tangpricha, Guy G T’Sjoen, Endocrine Treatment of Gender-Dysphoric/Gender-Incongruent Persons: An Endocrine Society Clinical Practice Guideline, The Journal of Clinical Endocrinology & Metabolism, Volume 102, Issue 11, 1 November 2017, Pages 3869–3903, https://doi.org/10.1210/jc.2017-01658
- ↑ https://www.sciencedirect.com/science/article/abs/pii/S0960076006001567
- ↑ Düsterberg, B., & Nishino, Y. (1982). Pharmacokinetic and pharmacological features of oestradiol valerate. Maturitas, 4(4), 315–324. https://doi.org/10.1016/0378-5122(82)90064-0
- ↑ Thurman, A., Kimble, T., Hall, P., Schwartz, J. L., & Archer, D. F. (2013). Medroxyprogesterone acetate and estradiol cypionate injectable suspension (Cyclofem) monthly contraceptive injection: steady-state pharmacokinetics. Contraception, 87(6), 738–743. https://doi.org/10.1016/j.contraception.2012.11.010
- ↑ Wiemeyer, J. C., Fernandez, M., Moguilevsky, J. A., & Sagasta, C. L. (1986). Pharmacokinetic studies of estradiol enantate in menopausic women. Arzneimittel-Forschung, 36(11), 1674–1677.
- ↑ Mayo Clinic. (Nov. 01, 2023). Bicalutamide (Oral Route) - Side Effects. Retrieved from https://www.mayoclinic.org/drugs-supplements/bicalutamide-oral-route/side-effects/drg-20072486?p=1
- ↑ Cockshott I. D. (2004). Bicalutamide: clinical pharmacokinetics and metabolism. Clinical pharmacokinetics, 43(13), 855–878. https://doi.org/10.2165/00003088-200443130-00003
- ↑ de Voogt H. J. (1992). The position of cyproterone acetate (CPA), a steroidal anti-androgen, in the treatment of prostate cancer. The Prostate. Supplement, 4, 91–95. https://doi.org/10.1002/pros.2990210514
- ↑ National Health Service. (6 July 2022). About Spironolactone. Retrieved from https://www.nhs.uk/medicines/spironolactone/about-spironolactone/
- ↑ 11.0 11.1 11.2 UCSF Transgender Care. (June 17, 2016). Feminizing hormone therapy. Retrieved from https://transcare.ucsf.edu/guidelines/feminizing-hormone-therapy
- ↑ Zito, P. M., Bistas, K. G., & Syed, K. (2022). Finasteride. In StatPearls. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK513329/#:~:text=2%5D%5B3%5D-,Finasteride
- ↑ Roehrborn, C. G., Lee, M., Meehan, A., Waldstreicher, J., & PLESS Study Group (2003). Effects of finasteride on serum testosterone and body mass index in men with benign prostatic hyperplasia. Urology, 62(5), 894–899. https://doi.org/10.1016/s0090-4295(03)00661-7
- ↑ Haverinen, A., Kangasniemi, M., Luiro, K., Piltonen, T., Heikinheimo, O., & Tapanainen, J. S. (2021). Ethinyl estradiol vs estradiol valerate in combined oral contraceptives - Effect on glucose tolerance: A randomized, controlled clinical trial. Contraception, 103(1), 53–59. https://doi.org/10.1016/j.contraception.2020.10.014
- ↑ "General information: Oestradiol valerate is equal to oestradiol 0.76 mg." ScienceDirect. Retrieved from https://www.sciencedirect.com/topics/neuroscience/estradiol-valerate#:~:text=General%20information%3A%20Oestradiol%20valerate%20is,equal%20to%20oestradiol%200.76%20mg
- ↑ Doll, Elizabeth E et al. “SUN-LB9 Pharmacokinetics of Sublingual Versus Oral Estradiol in Transgender Women.” Journal of the Endocrine Society vol. 4,Suppl 1 SUN-LB9. 8 May. 2020, doi:10.1210/jendso/bvaa046.2237
- ↑ Boston University School of Medicine. (2013). Practical Guidelines for Transgender Hormone Treatment. Retrieved from https://www.bumc.bu.edu/endo/clinics/transgender-medicine/guidelines/